"I saw a picture of myself when I came out of the hospital. I didn't recognize myself." - Amy Winehouse
Introduction
This gives you some idea of what happens and what to expect in the Hospital. Given that my research on the internet showed that the mortality rate for this operation at my age was now 25 percent my morale was not very high. I tried to console myself that a lot of operations were done when the patient was already very ill accounting for the high mortality.
For this hospital stay there were no visitors allowed. This is a hangover from Covid. My only communication with the outside world is telephone, email, whatsapp etc.
When going into hospital there are things to pack apart from the obvious essentials. For me these were:
A compact camera to record things.
A mobile phone
Do not bring precious items as with all the upsets and moves things can get mislaid. For example I could not find my electric razor for about six days but it eventually turned up.
Try to back up things, ie An electric razor and wet disposable razors. Two chargers for electrical items and cables to charge everything. For example my Kindle normally lasts four weeks so I did not bring a charging cable. With extra use in hospital after ten days it needed charging. I had to have a charging cable sent in to me.
The hospital provided wifi. It also provided a dedicated phone and phone number at the bedside.
Background
The hospital stay started on the 5th September 2022 and finished on the 23rd September 2022 a total of 18 days. On the 25th October 2022 I was signed off by the surgeon 6 weeks 5 days after operation as healthy. On the 12th October 2022 the heart specialist declared me as fit and healthy 5 weeks after operation.
Daily Regime
These are things that happen each and every day you are in hospital and are part of the daily routine.
Each day at around 11am there was a visit from the head of medicine and his team to every patient to discuss the case, treatment for the next day or so and ask how the patient is.
If you think you will get a good night's sleep then think again. Each night every two hours the nursing staff physically check each patient.
You have a monitor attached to you with about 5 wired sensors in different positions on you. It is a portable monitor that can be put in you pocket but it does require charging which tethers you when charging. The sensors do come detached especially at night when you move in your sleep. If this happens you are woken up to fix it.
Physical monitoring of blood pressure temperature etc. at least twice per day at about 6am and 9pm.
Normally you are weighed every day. You will lose weight. When I went into hospital I weighed 80.8kg (178 pounds). When I left 18 days later I weighed 74.9kg (165 pounds) so I lost 5.9kg (13 pounds). I believe this is about normal.
There is a written menu of food every day. The nutritionist visits everyday with various options for food for the next few days.
There are tests done almost every day such as Electrocardiogram (ECG), x-ray, ultrasound, MRI scan. Some are with portable equipment taken to your bedside and some you have to go and visit.
Monday 5th September 2022
Hospital Admission in the afternoon. This included a certificate from my dentist that my teeth are OK and not going to fall out during the operation. I was allocated Room 205 which I stayed in until the operation. I was weighed at 80.8kg (178 pounds). Various tests including X-ray and MRI scan were performed.
Tuesday 6 September 2022
Before the operation all body hair was removed by the nurses as it is considered a risk of infection. Coronary Artery Investigation was done via the femoral artery in the operating theater. This was to verify that there was no problem with my coronary artery that could jeopardize the operation. It was uncomfortable but not that painful.
Wednesday 7 September 2022
Lots More tests. These are all test to give more information to the surgeon and verify that my body stands a chance of surviving the operation.
Thursday 8 September 2022
Covered in yellow Antiseptic liquid as preparation for the operation, then moved to the operating theater. The operation started around 13:00 and its duration was approximately 2 hours. I was moved to the intensive care ward after the operation. I am completely out of it and do not remember a thing after being moved to the operating theater. Not surprising after what has been done.
Friday 9 September 2022
Still in the intensive care ward. I have a visit from my surgeon in the morning. I am almost completely out of it as I am on a Morphine drip and recovering from the anesthetic. The nurses change the dressing on my ribcage.
Saturday 10 September 2022
Started the day in the Intensive care ward. I was transferred in the afternoon to a normal ward and room 201 which does not change for the rest of my stay. I am more awake and not really in pain as the Morphine helps.
Sunday 11 September 2022
Blood pressure is 160 which is high. The nurses change the dressing on my ribcage. They decided to leave the drainage tubes from the operation in place and review it Monday. These are attached to me and a reservoir under the bed effectively chaining me to the bed. Sunday night I had an attack of tachycardia. It was weird almost like I was hallucinating. Thankfully at about 2am a nurse came and brought me medication which calmed things down. Apparently it's quite common after a heart operation but usually settles down.
When you are attached to the bed organization of what you need is very important. You need to have everything within reach as you cannot just get out of bed to get it.
After the operation there is pain management. Initially morphine, it is a morphine perfusion. I had the morphine stopped as I complained of nausea, which is one of the side effects. Afterwards it is just paracetamol on request. It is always a good idea to take some before the the physiotherapist arrives.
You are ordered to drink lots of water each day and they measure your consumption and force more on you if you are not drinking enough. For urinating when attached to a bed, a bottle is the only solution. You have to make sure it is available at all times as you will get caught short. for a period after the operation a catheter handles this again with a reservoir under the bed which attaches you to the bed.
Monday 12 September 2022
Blood pressure is now 130 which is much better. They decided to remove the drainage tubes from the operation but then found a blood clot blocking one of them. They put everything back and will wait till Tuesday. Also today I had a problem with diarrhoea. Diarrhoea is not pretty when you are attached to the bed and cannot move.
Tuesday 13 September 2022
Blood pressure is now 120 which is normal. The nurses change the dressing on my ribcage. Today they decided to remove almost everything and by Tuesday evening I only had the monitoring and was almost mobile. They even removed the catheter. The night nurse then tells me if I do not produce liquid within 2 hours she will have to put the catheter back. Often in men the muscle closing the bladder becomes paralyzed with a catheter. She gave me a muscle relaxant and within 20 minutes I had produced half a liter. I slept very well Tuesday night. My blood pressure Wednesday morning was down to 110 from 160 previous mornings.
Things fixing you to the bed
Monitoring devices all the time from admission to discharged. These are attached at five or six points on the body. they often come loose and rsult in the nurse coming to fix them back on again. You can be semi mobile with the monitoring as it is a battery pack you carry and only needs a link to charge as the connection is wifi. Infusions after operation for morphine, saline, several drugs, anti-biotics. Again can be semi mobile as it is on a pole with wheels. drainage tubes inserted during the operation and for several days afterwards with a resevoir under the bed. A catheter is inserted during the operation and left for several days with a resevoir under the bed. As they administer so much and take blood samples multiple times a day then semi permanent access points are inserted in shoulders, wrists, etc so they can have a choice if one does not work well.
Wednesday 14 September 2022
Blood pressure is now 110 which is completely normal. They believe I have a bacterial infection and have put me on antibiotics. They have taken samples of everything, saliva, blood, urine, fecal matter etc. for analysis. I am very tired but making progress. Wednesday night the diarrhoea returns.
There are tests every day, ECG, ultrasound, x-ray, blood tests, urine tests, MRI scans. Medication there are at least 15 different pills each day, injections, infusions, taking of blood. Nurses take blood pressure, heart rate, oxygen level, temperature at least 4 times per day.
Thursday 15 September 2022
Blood pressure is 120, normal again The nurses change the dressing on my ribcage. The diarrhoea is worse this morning They are giving me antibiotics as a perfusion. At midday they give me Imodium and I slept all afternoon. So far they have found nothing dangerous but they are waiting on results for variants of one bacteria they found.
Friday 16 September 2022
Blood pressure is 120 over 70. I am much better but lacking energy. They are keeping me in at least till Monday.
Saturday 17 September 2022
Blood pressure is 140, slightly up. The nurses change the dressing on my ribcage. Today is my planned day to leave hospital but as I have a bacterial infection they are holding me until one the infection is identified and that it is completely gone. This is because it can undo all the good work they have done with the operation. They have finished with the current antibiotics, taken lots of blood and wait for results that the bacteria are gone. It looks like earliest Tuesday for leaving.
Sunday 18 September 2022
Blood pressure is 110 over 70. I am weighed at 76.1kg (168 pounds). They have identified the bacteria (Staphylococcus Lugdunensis) and it is dangerous as it can cause aggressive endocarditis. They have hooked me up to a perfusion of targeted antibiotics (Cefazolin) to kill it. No indication yet of how long it will take. Ultrasound scan says valve is opening and closing correctly with no reflux. Also after the operation the liquid below my heart has now gone.
I am now over my planned leaving date and running out of clean pajamas, underwear and toiletries. My kindle reader which normally lasts four weeks is now out of charge and I did not bring a cable to charge it. I need shower gel and shampoo as they decided to leak in my toiletries bag leaving me with none. One quick phone call and my partner puts another bag together and delivers it the hospital and it gets delivered to me as no visitors are allowed. The no visitors is a hangover from Covid.
Monday 19 September 2022
Blood is pressure 140. I am weighed at 75.1kg (166 pounds). They do an ultrasound scan of my ribcage. An infection specialist visits and says if I have a fever or infection after I leave hospital to think of my heart and take a blood test. Today all the infusions were removed so I am mobile and not chained to the bed. The nurses change the dressing on my ribcage. They have removed the wires for the pacemaker which were put in during the operation.
Tuesday 20 September 2022
Blood pressure is 130 and heart rate 80bps I am weighed at 75.4kg (166 pounds). At the daily briefing they give Thursday as my earliest hospital leaving date
Wednesday 21 September 2022
Blood pressure is 120. I am weighed at 74.9kg (165 pounds). I am constipated so they give me 20g of Forlax a laxative. The leaving date is now Friday. They Want me to finish the course of antibiotics while I am at the hospital. The nurses change the dressing on my ribcage.
Thursday 22 September 2022
Blood pressure is 125 and heart rate 72bps. At 16:00 I have my first bowel movement in a week.
Friday 23 September 2022
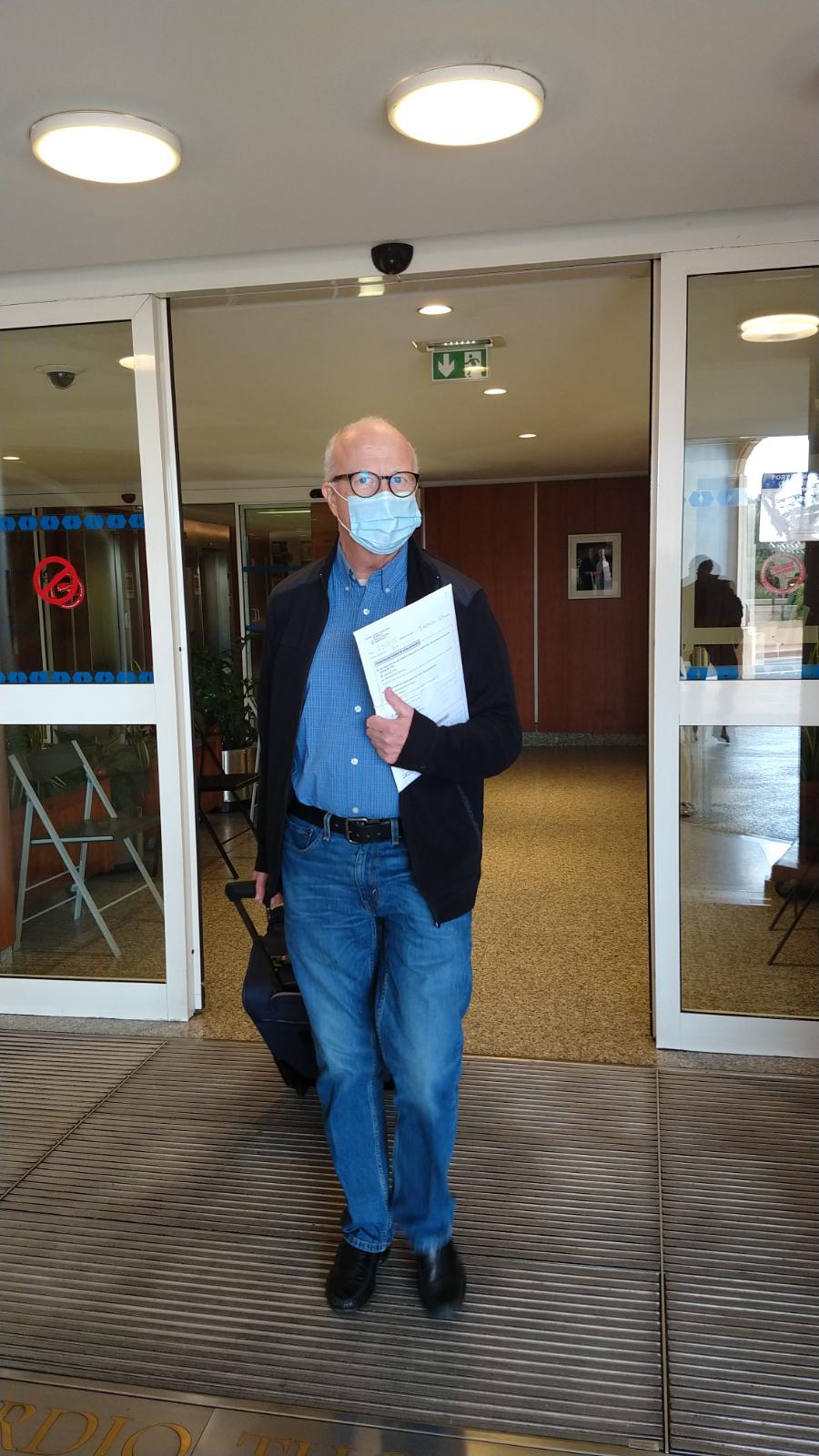
Blood pressure is 130 slightly raised in anticipation of me leaving. The nurses change the dressing on my ribcage. I am discharged from the hospital at about 12:30pm with lots of documents about diets and after care.